Why do we replete potassium to >4.0?
One of the most common orders placed by inpatient doctors is supplemental potassium chloride in the setting of hypokalemia. Although most don’t learn it in the preclinical years, once a student has spent more than a few hours on the wards they realize nearly everyone repletes the serum potassium to >4.0 mEq/L.
Whether we know it or not, repleting potassium to >4.0 mEq/L is largely aimed at preventing ventricular arrhythmias (i.e., ventricular tachycardia and ventricular fibrillation). With very low values (e.g., <2.5 mEq/L) more generalized muscle weakness can also occur, this degree of hypokalemia is far rarer.
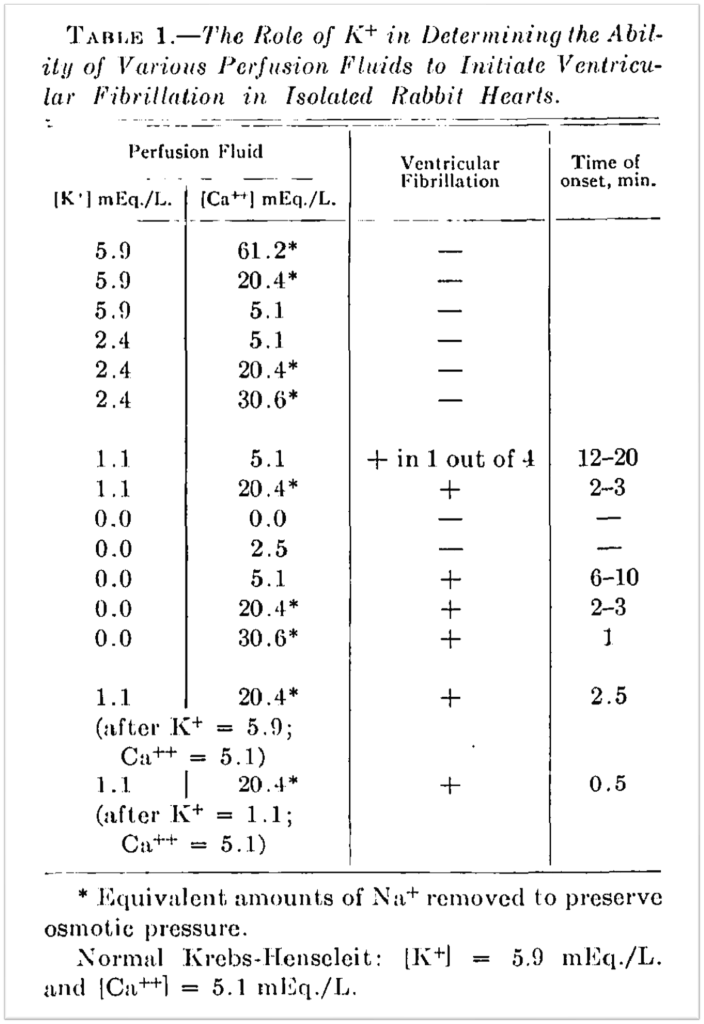
The early evidence for potassium repletion comes from animal studies showing that infusion of low-potassium fluid causes ventricular fibrillation. For example, in 1954 Grumbach, Howard, and Merrill observed that infusion of low-potassium fluid caused ventricular fibrillation in rabbit hearts. Interestingly, this was not seen if the potassium concentration was ≥2.4 mEq/L or if calcium was absent. Even if the serum potassium was 0, VF didn’t occur unless calcium was present.
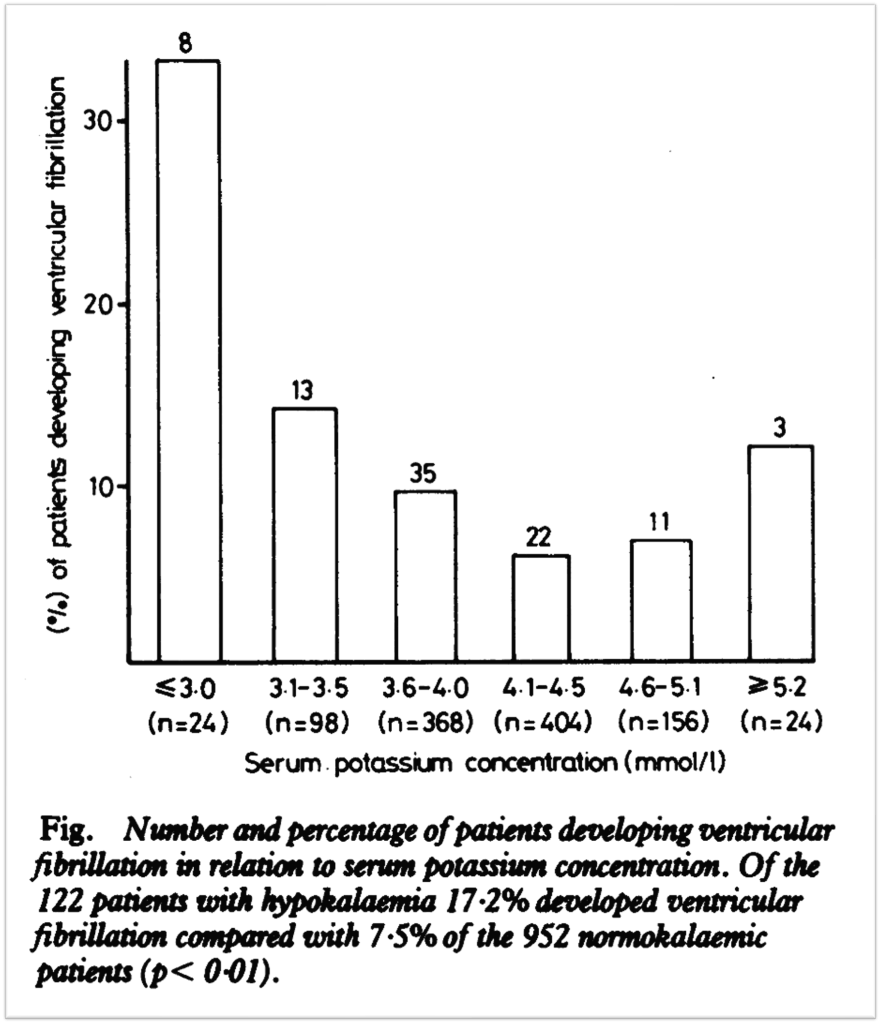
Over the next few decades, observational studies showed that in patients with acute myocardial infarction, a potassium <4.0 mEq/L was associated with ventricular arrhythmias. Because we don’t have RCT data supporting or refuting the benefit of repleting patients with acute MI to a particular value, early guidelines generally erred on the side of caution and suggested we keep patients above 4.0.
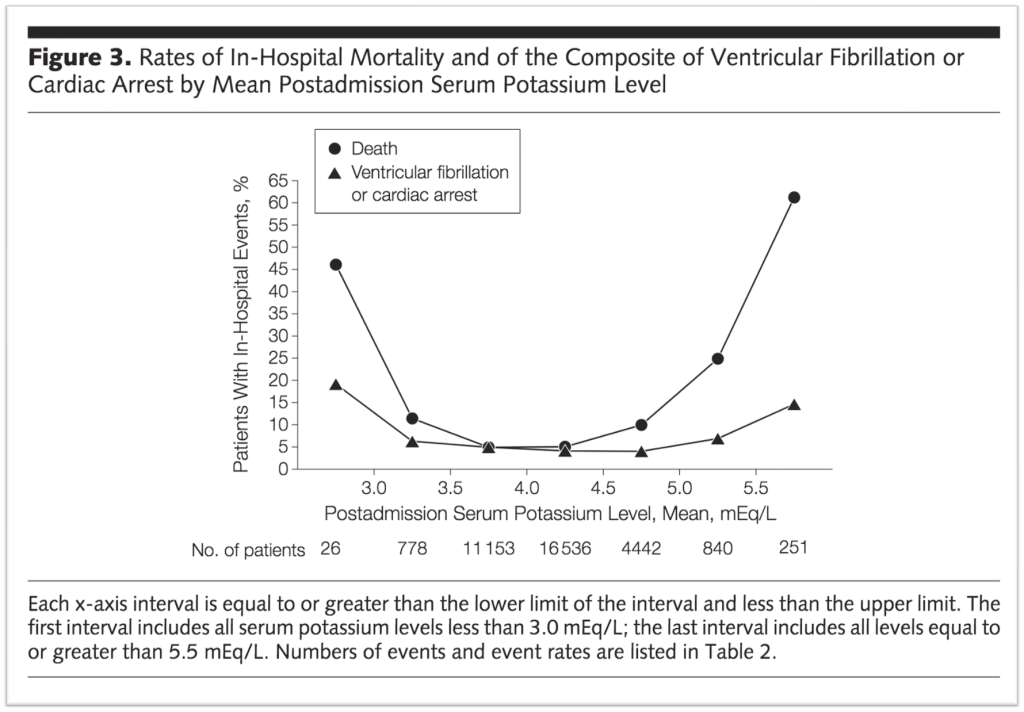
More recent data supports a slightly lower goal serum potassium. A 2012 study published in JAMA looked at over 38,000 patients with acute MI. The rates of in-hospital mortality and in-hospital ventricular fibrillation or cardiac arrest were flat between 3.5 and 4.5 mEq/L.
For patients with heart failure, there is variable evidence but most support a goal of greater than 4.0 mEq/L. Then there are other conditions, like cirrhosis with risk of hepatic encephalopathy where a higher target may also make sense. Lower serum potassium enhances renal ammonia generation resulting in an increase in serum ammonia levels. And there is some data suggesting that patients with hepatic encephalopathy improve more quickly if they have a higher potassium. So, it seems reasonable to keep them above 4.0 mEq/L.
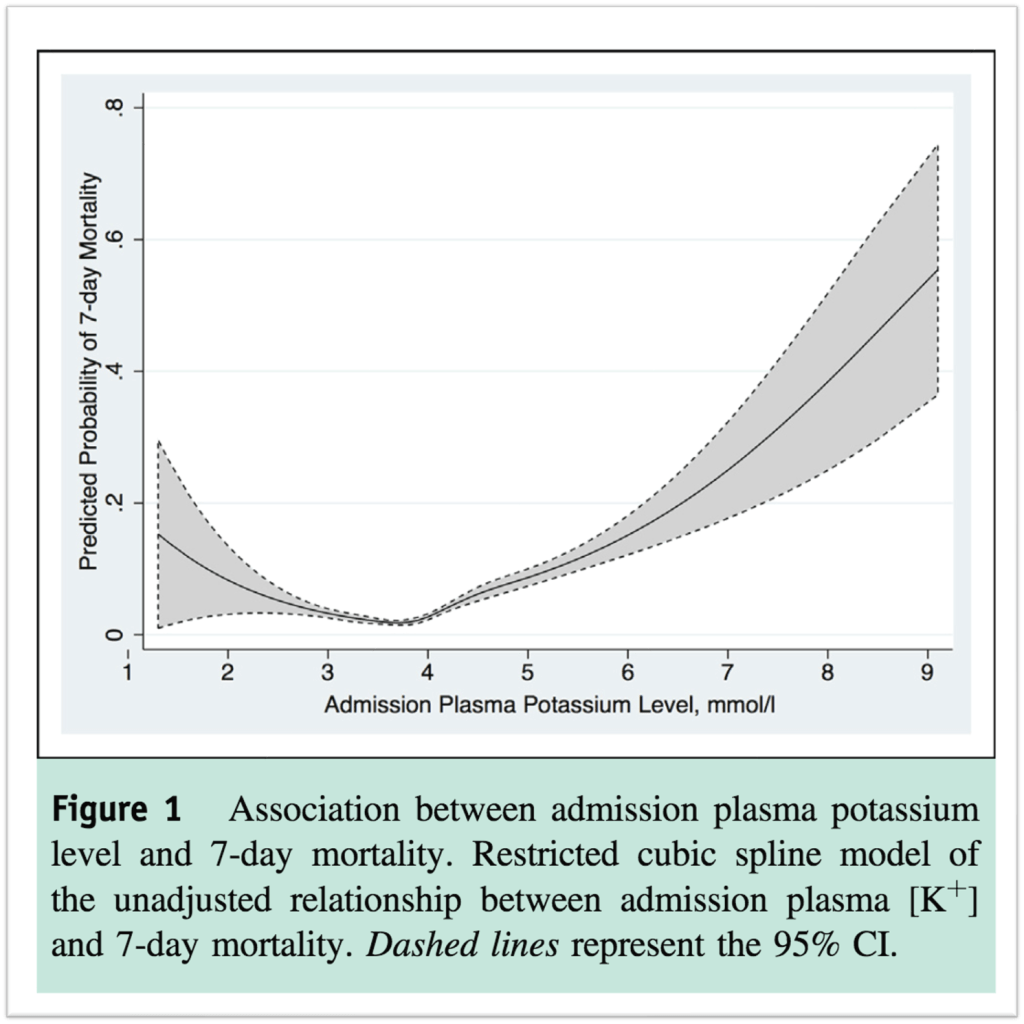
As for other patients, there is some observational data but it isn’t as robust as the data for acute MI. One study published in 2015 in the American Journal of Medicine looked at about 12,000 hospitalized with an acute medical condition. Seven-day mortality didn’t rise until potassium fell fellow 2.9 mEq/L.
Another study published in 2019 found that patients who were successfully repleted to ≥3.5 mEq/L had no reduction in rates of arrhythmia. In fact, patients with an arrhythmic event received a statistically significant higher amount of potassium.
Repleting potassium to greater than 3.5 mEq/L or 4.0 mEq/L assumes two things. First, it assumes that hypokalemia causes ventricular arrhythmias. Second, it assumes that increasing potassium via supplementation will mitigate that risk. There is almost no data supporting the second assumption. Even the first assumption can be called into question.
It could be that hypokalemia does not cause ventricular arrhythmias. Instead, another factor could be causing both hypokalemia and VT/VF. For patients with acute myocardial infarction that other thing might be epinephrine.
We know that epinephrine activates β2 receptors leading to increased activity of the Na/K-ATPase. This results in the movement of potassium into cells and a drop in serum levels.
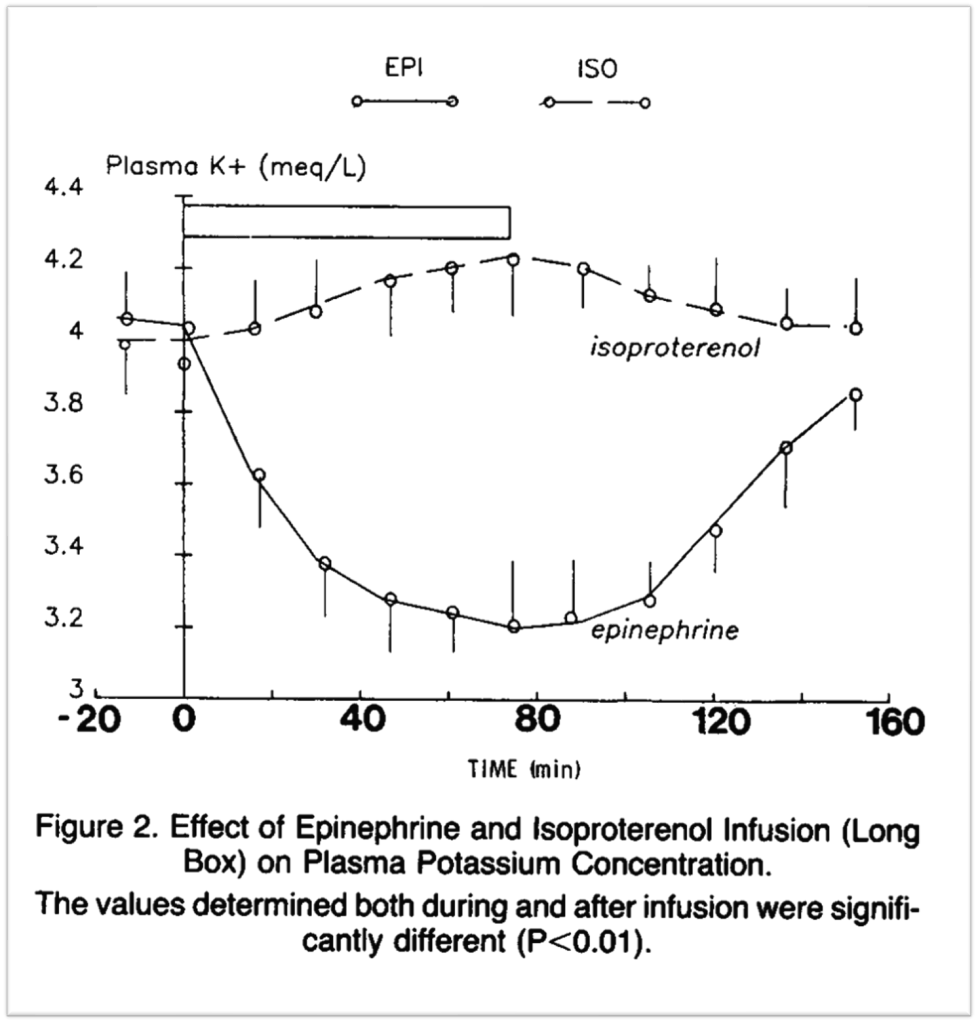
Many studies have found that higher levels of catecholamines are associated with ventricular tachycardia and fibrillation in patients with acute MI. And there is a strong consensus that this is a causal relationship. And, the benefit of β-blockers in acute MI may be partly related to their ability to blunt catecholamines.
Now, of course, β-blockers can blunt the decrease in potassium specifically seen with epinephrine. In fact, most of the medications which have a mortality benefit in acute MI and heart failure increase potassium. β-blockers, ACE inhibitors, ARBs, and aldosterone antagonists all-cause higher serum potassium. That all these medications increase potassium is intriguing but far from definitive proof that hypokalemia causes ventricular arrhythmias.
Still, despite the alternate explanation discussed above, ultimately there is a very strong case that there is a direct causal link between hypokalemia and ventricular arrhythmia. But it also seems that you need other factors like a sensitive myocardium – as seen in acute MI – or a proarrhythmic milieu, something high levels of epinephrine provide.
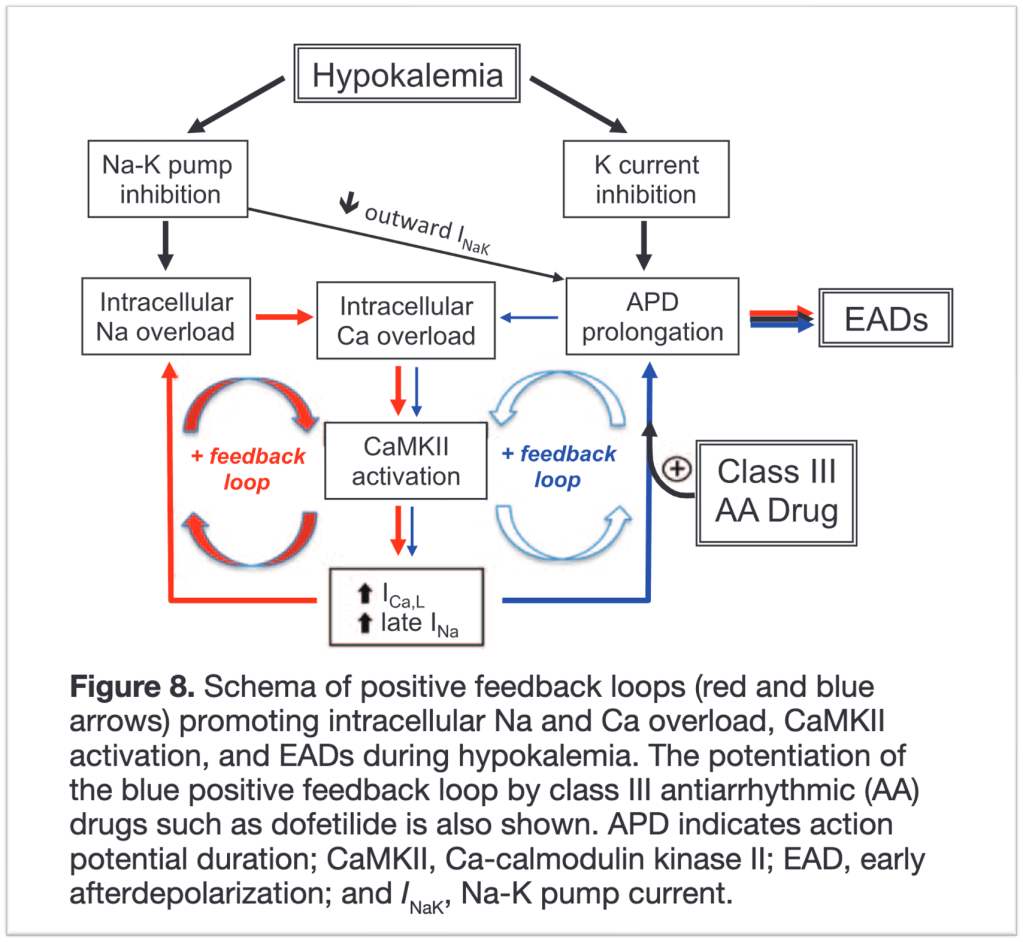
There are a number of potential mechanisms. One begins with decreased activity of the Na/K-ATPase. With low serum potassium, there is less of a drive to move potassium into cells. So the Na/K-ATPase is less active. This has been shown in rat myocytes.
When this happens, the intracellular sodium concentration rises in parallel. This leads to decreased activity of the Na/Ca exchanger and increased intracellular calcium. The increased intracellular calcium concentration leads to increased Ca-calmodulin kinase II activity. Eventually, this can result in early afterdepolarization-mediated ventricular arrhythmias.
Taken together, the best available data supports maintaining potassium values above 3.5 mEq/L in patients with acute MI, though a more conservative goal of 4.0 mEq/L can be argued for as well. For heart failure, 4.0 mEq/L is well supported. Aiming for a higher value, whether that is 3.5 mEq/L or 4.0 mEq/L in patients with cirrhosis, particularly when they have hepatic encephalopathy, seems appropriate though there are fewer data available for this patient population.
For other patients, a target of at least 3.0 mEq/L could be supported. It may be valuable to see if hypokalemia persists without repletion. If it does, we should ask why? Does the patient have alcohol withdrawal and increased catecholamines causing hypokalemia? Do they have hypertension and this is a clue that they have increased aldosterone levels? Instead of reflexively repleting we should pause for a moment and ask why the potassium is low in the first place.
Take Home Points
- The goal potassium of ≥4.0 mEq/l likely derived from studies of AMI
- A more appropriate range for these patients may be 3.5-4.5 mEq/L
- Repleting all hospitalized patients to >4.0 mEq/L is less evidence-based
- Hypokalemia may lead to VT/VF via the reduced function of the Na/K-ATPase
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (0.5 hours), Non-Physician Attendance (0.5 hours), or ABIM MOC Part 2 (0.5 hours).
Listen to the episode
https://directory.libsyn.com/episode/index/id/23503604
Credits & Citation
◾️Episode and show notes by Tony Breu
◾️Audio edited by Clair Morgan of nodderly.com
Breu AC, Abrams HR, Cooper AZ. Replete with Kare The Curious Clinicians Podcast. June 22, 2022.