Why do we use ACE inhibitors to treat scleroderma renal crisis?
In a day of seeing adult patients in any type of clinic, it’d be hard to not hear the words “ACE inhibitor” at least once. Since the introduction of captopril in the mid-1970s and subsequent family members like lisinopril, ACE inhibitors have been game changers in controlling blood pressure, preventing cardiac remodeling, and protecting renal function. We tend to think of ACE inhibitors, therefore, as drugs for hypertension, heart failure, and diabetic kidney disease. However, their greatest pound-for-pound benefit may actually have been in the treatment of a rare disease that, prior to the 1970’s, was considered universally fatal: scleroderma renal crisis.
First, a brief primer on scleroderma and scleroderma renal crisis. Scleroderma is an autoimmune disease characterized by unchecked fibrosis of endothelial surfaces, particularly on microvasculature. In localized scleroderma, the effects are mostly on skin and subcutaneous tissue. In systemic scleroderma, or systemic sclerosis (SSc), fibrosis of organs such as the esophagus, pulmonary arteries, and kidneys is seen. Scleroderma renal crisis is a dangerous complication that affects 2-15% of those with SSc. It presents abruptly with hypertension, elevated creatinine, oliguria with a normal urinalysis, and in 50% of patients, microangiopathic hemolytic anemia, in which platelets abnormally aggregate and shear red blood cells.
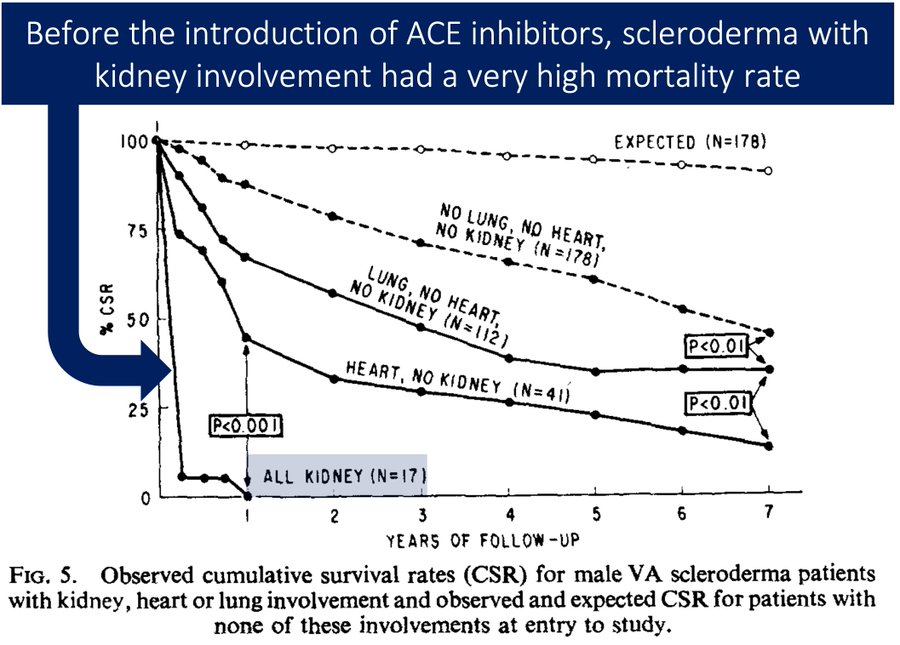
Before the introduction of ACE inhibitors, scleroderma renal crisis was a virtual death sentence. In a 1973 study of 358 male veterans with SSc, all 17 patients with renal involvement at entry died within 10 months, with only one living past 3 months. Although hemodialysis has been around since the 1940s, it is not effective by itself. In one 1978 study of 25 patients with scleroderma renal crisis, 8 out of 8 patients who didn’t undergo dialysis died within 6 months, but 9 out of 10 patients who did get dialysis still died within the same timeframe.
In this same study, however, one group did have increased survival: 4 out of 9 patients who got hemodialysis as well as a bilateral nephrectomy. This is counterintuitive: treating worsening kidney failure by causing the ultimate kidney failure. However, the mechanism behind this drastic treatment is the same one that makes ACE inhibitors so effective in treating renal crisis.
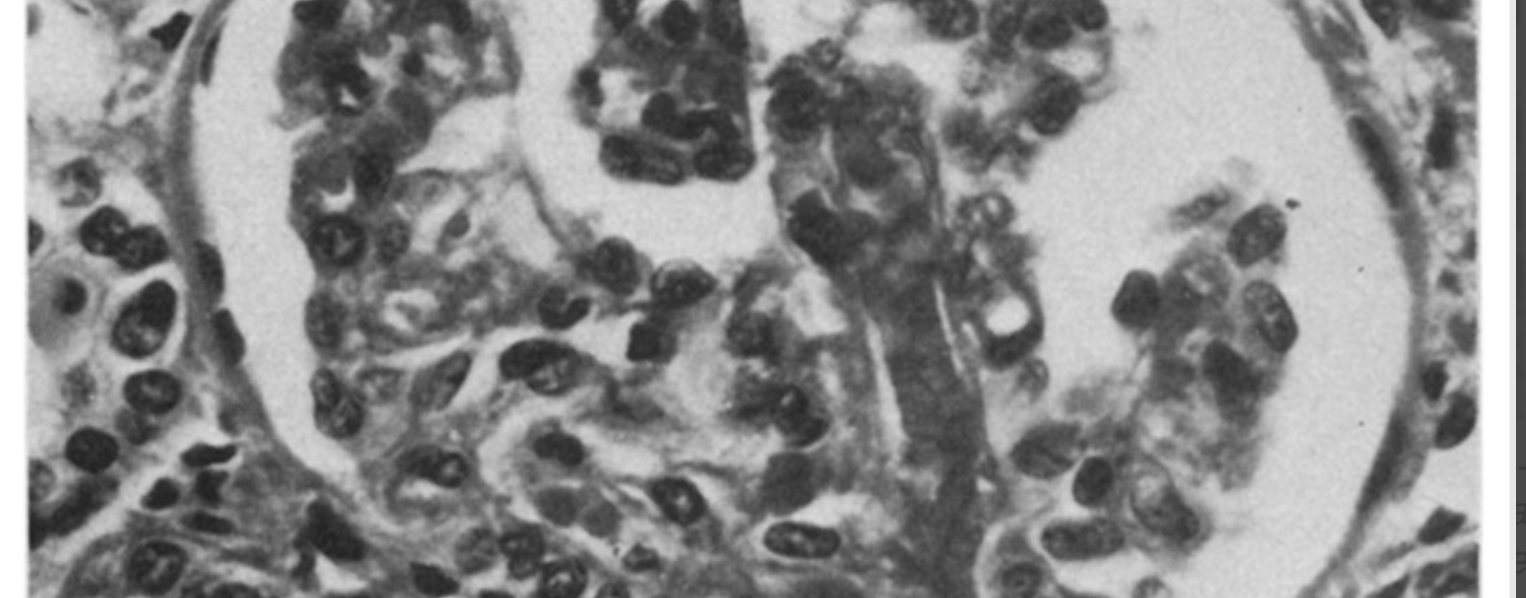
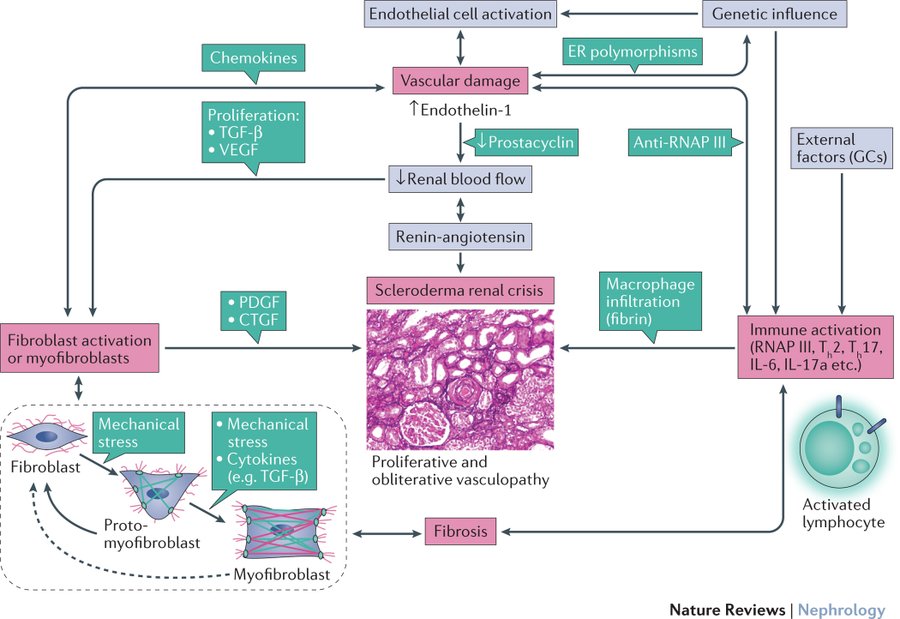
Scleroderma causes endothelial damage in the renal vasculature. This decreases perfusion to the kidneys, which causes the juxta-glomerular apparatus (JGA) to undergo hyperplasia. The JGA is the calibrator of the kidney: it releases renin to vasoconstrict the afferent and efferent arterioles of the kidney to adjust perfusion accordingly, as well as stimulate vasoconstriction throughout the body. The less perfused the kidneys are, the more renin they release. In scleroderma renal crisis, the JGA releases huge amounts of renin without any feedback inhibition, leading to increased activation of the renin-angiotensin-aldosterone system (RAAS) and uncontrollable hypertension. By removing the kidneys, the source of renin is also removed.
The presence of elevated renin in scleroderma renal crisis was noted in the late 1970s, just before bilateral nephrectomies were noted to improve survival. The first ACE inhibitor, captopril, was synthesized in 1974. ACE inhibitors work by blocking a key step in RAAS, the conversion of angiotensin I to angiotensin II (an interesting aside: captopril is an analog of the venom of the Brazilian viper Bothrops jararaca, whose bite causes victims to collapse, which researchers hypothesized was due to venom-induced hypotension.) It made sense, then, to try treating a disease of excess renin with a drug that can mute its effects. In 1979 (a year after the nephrectomy study), the first case report of two SSc patients successfully treated with captopril was published.
Larger studies have since supported ACE inhibitors’ protective effects. In a 1990 cohort study of 108 patients with renal crisis, those receiving treatment had a 1-year survival of 76%, compared to the 15% survival of those who did not receive treatment. It should be noted that ACE inhibitors are not a panacea: in the same study, 44% of those treated still either died early or required permanent dialysis. However, the positive effect of ACE inhibitors on scleroderma renal crisis morbidity and mortality is incontrovertible.

Other drugs that either reduce renal production of renin (like β1 blockers) or block renin itself (like aliskiren) have been tried for scleroderma renal crisis. In the case of the former, early, pre-captopril case reports were promising, but they are no longer recommended due to the potential for vasospasm. In the case of the latter, no controlled trials have compared it to ACE inhibitors. The pathophysiology of scleroderma renal crisis is probably more complex than just renin: endothelin-1 (another vasoconstrictor) may also be elevated, and bosentan, an endothelin-1 receptor antagonist most known for treating pulmonary hypertension, has shown promising results. For now, however, ACE inhibitors remain the “ace” treatment for scleroderma renal crisis.
Take Home Points
- The use of ACE inhibitors (ACEi) has resulted in greatly improved survival in scleroderma renal crisis (SRC).
- SRC is associated with markedly elevated renin levels.
- ACEi address the downstream vasoconstriction seen in the setting of elevated renin.
Link to Related Tweetorials
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (0.5 hours), Non-Physician Attendance (0.5 hours), or ABIM MOC Part 2 (0.5 hours).
Listen to the episode
https://directory.libsyn.com/episode/index/id/28551515
Credits & Citation
◾️Episode written by Tony Breu
◾️Show notes written by Giancarlo Buonomo and Tony Breu
◾️Audio edited by Clair Morgan of nodderly.com
Breu AC, Cooper AZ, Abrams HR. Scleroderma Renal Crisis. The Curious Clinicians Podcast. November 8, 2023.
Image Credit: Stone RA, Tisher CC, Hawkins HK, Robinson RR. Juxtaglomerular hyperplasia and hyperreninemia in progressive systemic sclerosis complicated by acute renal failure. Am J Medicine 1974;56(1):119–23.