How does sickle cell trait protect against malaria infection and mortality?
In any medical genetics course, sickle cell trait (SCT) and sickle cell disease (SCD) are sure to be brought up early and often. They follow an easily-understood inheritance pattern and can be used as examples in teaching biochemistry basics such as protein folding and the function of hemoglobin. At the end of such lessons, this “fun fact” is invariably thrown in: SCT helps protect against malaria. This makes a certain amount of sense both evolutionarily and epidemiologically. Since SCD has such high morbidity, there must be a reason that the prevalence of sickle-cell trait is 30-40% in the areas of Africa with the highest rates of malaria transmission. What’s the biology behind this?
Let’s start with hemoglobin. Every red blood cell (RBC) contains ~280 million of these iron-containing metalloproteins, and the average human has 1.7 pounds of it. The normal Hemoglobin A (Hb A) is made of 4 protein subunits: two alpha globins and two beta globins. Each person has a gene (and two alleles) for the alpha and beta globins separately. In sickle-cell trait, one allele for beta globin is mutated such that a glutamic acid is replaced by valine. This mutated beta globin has a hydrophobic residue which, under conditions of low oxygen or dehydration, can stick to other beta globins, causing the whole RBC to deform into a sickle shape.
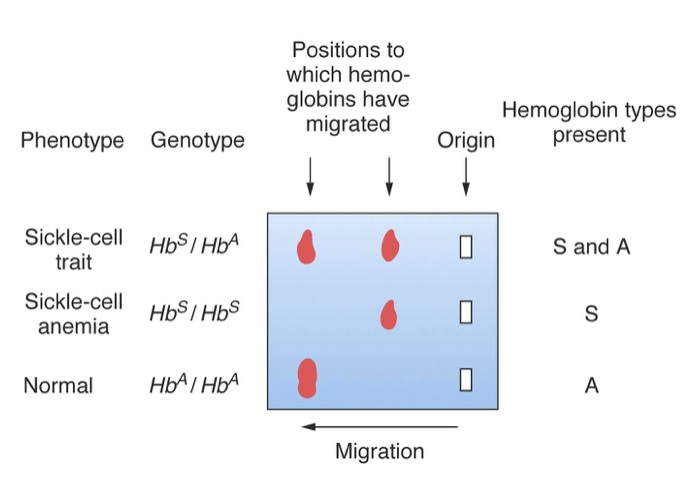
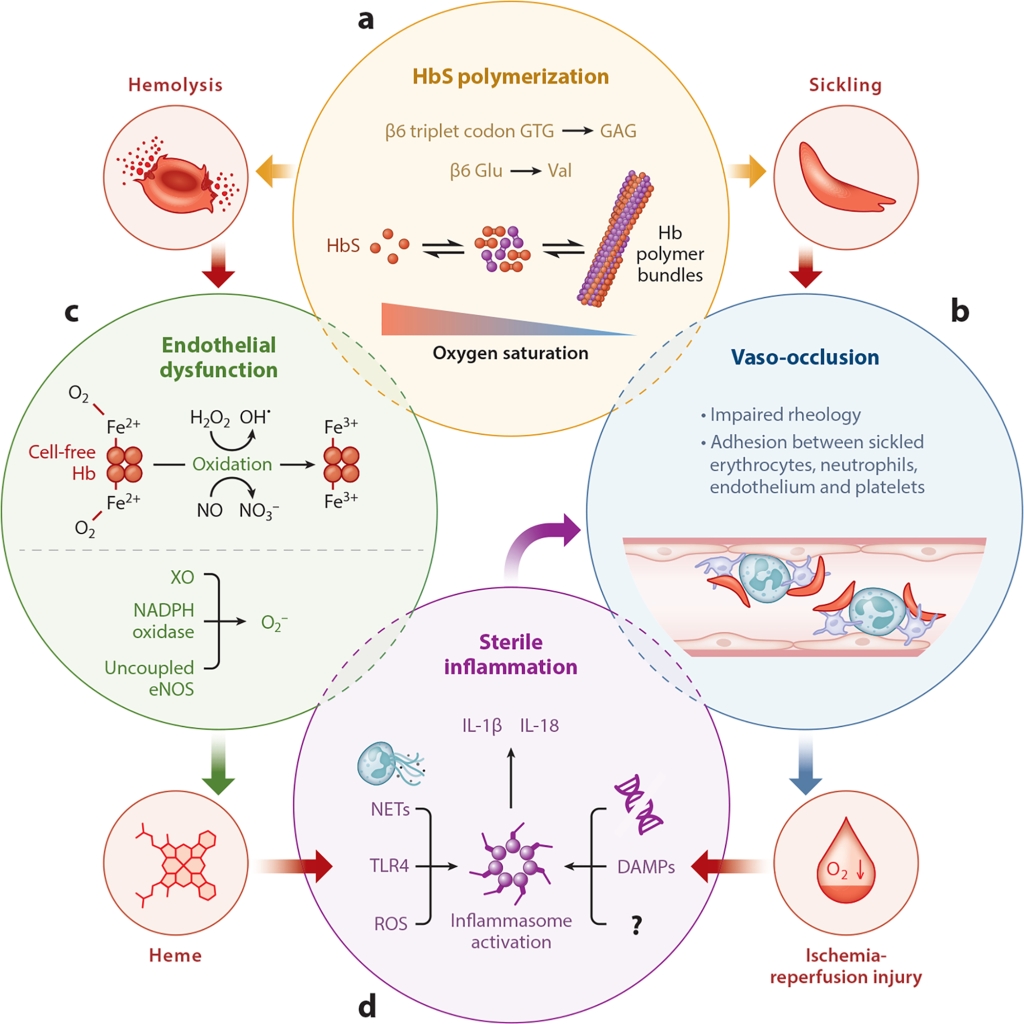
In SCT, the person still has one normal allele, and is able to produce enough functional beta globin to be unaffected unless they are in extremes of low oxygen or acidemia like scuba diving, high-altitudes or prolonged exercise. In sickle cell disease (sometimes called sickle cell anemia), individuals only have the mutated beta globin, giving them Hemoglobin S (Hb S). All the RBCs of someone with Hb S are prone to aggregate and sickle, especially in the narrow arterioles and capillary beds of the lungs, spleen and limbs. This causes complications such as painful vaso-occlusive crises, splenic auto-infarction, and acute chest syndrome. SCD is an autosomal recessive condition, meaning both alleles must be abnormal for the disease to manifest. Therefore, the child of two asymptomatic parents who are carriers for Hb AS has a 25% chance of having SCD.
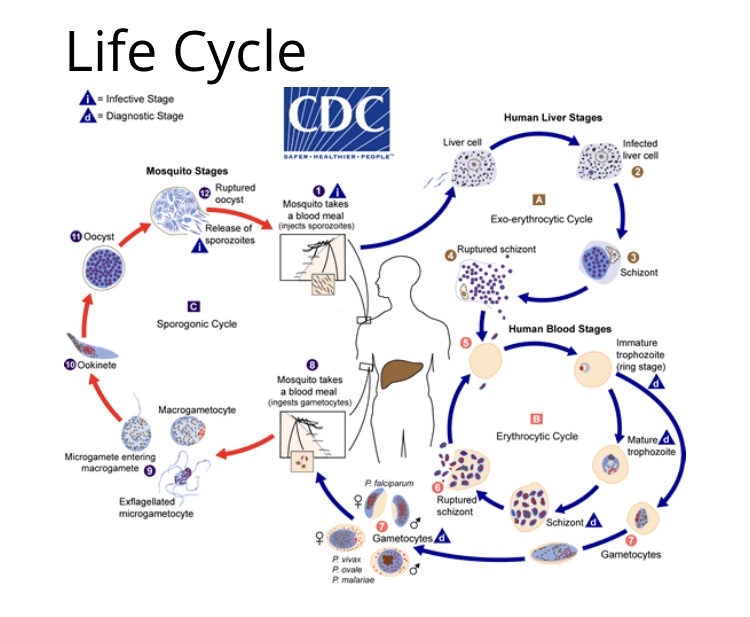
Malaria is, like SCD, a disease of RBCs. Anopheles mosquitoes bite humans and infect them with sporozoites, immature forms of the Plasmodium parasite. These sporozoites go to the liver, where they multiply and develop into schizonts, until finally lysing the hepatocyte and entering the bloodstream. The mature Plasmodium parasites can then infect RBCs, multiplying more before also bursting them. One of the life-threatening complications of malaria, therefore, is severe hemolytic anemia. Malaria (from the Italian mal aria or “bad air,” as it was once believed to come from noxious fumes) is one of the oldest diseases known to mankind, and still one of the most devastating. According to Unicef, in 2021, there were 250 million cases of malaria globally, with 619,000 deaths, and more than 75% of these were children under 5.
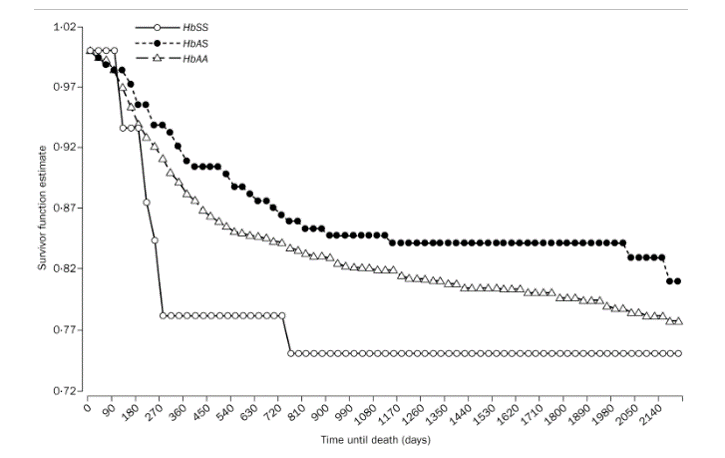
In 1954, South African physician Anthony Allison posited that the sickle cell gene had persisted in certain populations because it protected against both malaria infection and mortality even if infected. He inoculated volunteers with Plasmodium falciparum to striking results: 14/15 without sickle-cell trait developed parasitemia, while only 2/15 with the trait did. The conclusions from this data are supported by larger, more recent studies. One 2002 paper followed 1,000 children in Ethiopia from birth and found that sickle cell trait was protective against all-cause mortality, high-density parasitemia and severe malarial anemia, especially between the ages of 2-16 months when children are most susceptible to malaria. Other studies have also shown that sickle cell trait protects against cerebral malaria as well.
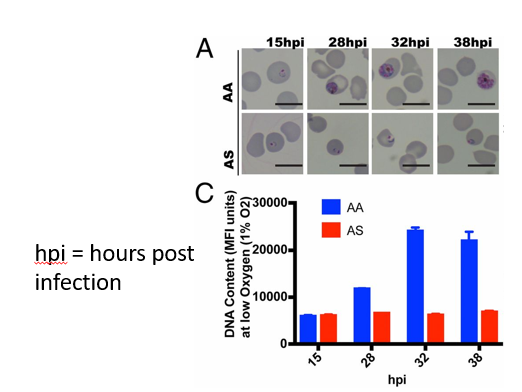
How does this happen? There are four basic mechanisms at play. In someone with sickle cell trait, Plasmodium infection causes RBC to sickle approximately 8x more than uninfected cells. These deformed RBCs are cleared by the spleen, which also eliminates the parasite. Chronic sickling and splenic clearance is what causes splenic ischemia and infarction in SCD. In this case, though, the sickling is actually beneficial in limiting infection.
The second mechanism builds on this propensity of Hemoglobin S to sickle when an RBC is infected with malaria. While in the “blood stage,” Plasmodium feeds itself via a protease that breaks hemoglobin down into digestible amino acids. When hemoglobin S polymerizes and sickles, this blocks the protease from degrading hemoglobin, depriving the parasite of nourishment.
These first two mechanisms assume that the RBC has already been infected with Plasmodium. As one 1992 study showed, patients with sickle cell trait may also have a heightened immune response against initial infection. The researchers took blood samples from children both with and without sickle cell trait at different times of the year, including malaria season. They then measured the lymphoproliferative response to malaria antigens introduced in vitro. The samples from sickle-cell trait patients during malaria season showed a heightened response, whereas the children without sickle cell had no seasonal change in response. This implies that patients with sickle-cell trait are better able to mount immune responses during the highest-risk periods for malaria.
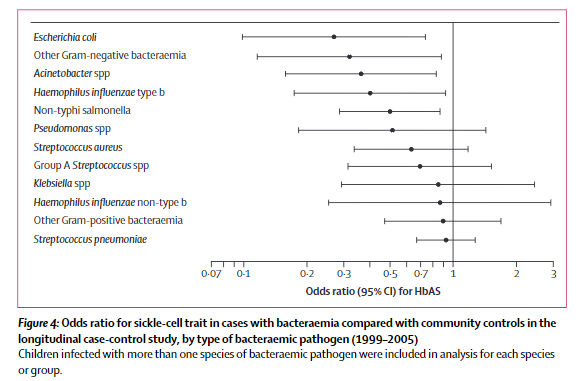
Although anemia and end-organ damage are the most well-known effects of malaria, bacteremia is also a significant cause of morbidity and mortality. One 2011 study studied malaria-related bacteremia among children 13 and under in Kenya. Malaria accounted for >50% of all cases of bacteremia in the geographic areas studied. At the same time, children with SCT had ⅓ the incidence of bacteremia compared to children without sickle cell trait. SCT seems to protect against both malaria infection and the worst consequences once infected.
Genetic analyses place the origins of the sickle cell gene around 7,300 years ago in Northern Africa. Although this area is now mostly occupied by the Sahara desert, several millennia ago it was the era of the “Green Sahara.” This wet, forested region was presumably plagued by malaria, and the novel mutation likely brought the individual in whom the mutation arose added protection, and therefore helped them survive childhood. The gene was then passed down through the generations. At the same time, the emergence and persistence of this mutation, so protective against malaria, also caused the emergence of sickle cell disease. This is an example of balancing selection.
Take Home Points
- Sickle cell trait protects against malaria infection and severe malaria manifestations if infection occurs
- This results from sickling within infected red blood cells, which leads to enhanced parasite clearance in the spleen, impaired parasite growth, and seems to be associated with enhanced anti-malarial immune responses
- Sickle trait also is associated with a significantly lower risk of secondary bacteremia resulting of malaria infection
Link to Related Tweetorials
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (0.5 hours), Non-Physician Attendance (0.5 hours), or ABIM MOC Part 2 (0.5 hours).
Listen to the episode
https://directory.libsyn.com/episode/index/id/28951123
Credits & Citation
◾️Episode written by Avi Cooper
◾️ Show notes written by Giancarlo Buonomo and Avi Cooper
◾️Audio edited by Clair Morgan of nodderly.com
Breu AC, Cooper AZ, Abrams HR. Avoiding Malaria. The Curious Clinicians Podcast. November 24, 2023.
Image credit: BSIP SA/Alamy Stock Photo

