In this episode of the podcast we explored why transmural myocardial infarctions cause ST elevations on EKG. While the it seems obvious that STEMIs are associated with ST elevations, the mechanism involved is fascinating and leads to doubts about the name!
To begin, recall that the ST segment represents the isoelectric period between depolarization and repolarization of the cardiac myocytes where there is no flow of charge (note that there are other periods which normally isoelectric, including the PR and TP segments). There is no net flow of charge after the end of depolarization (marked by the end of the QRS) and until the beginning of repolarization (marked by the beginning of the T wave).
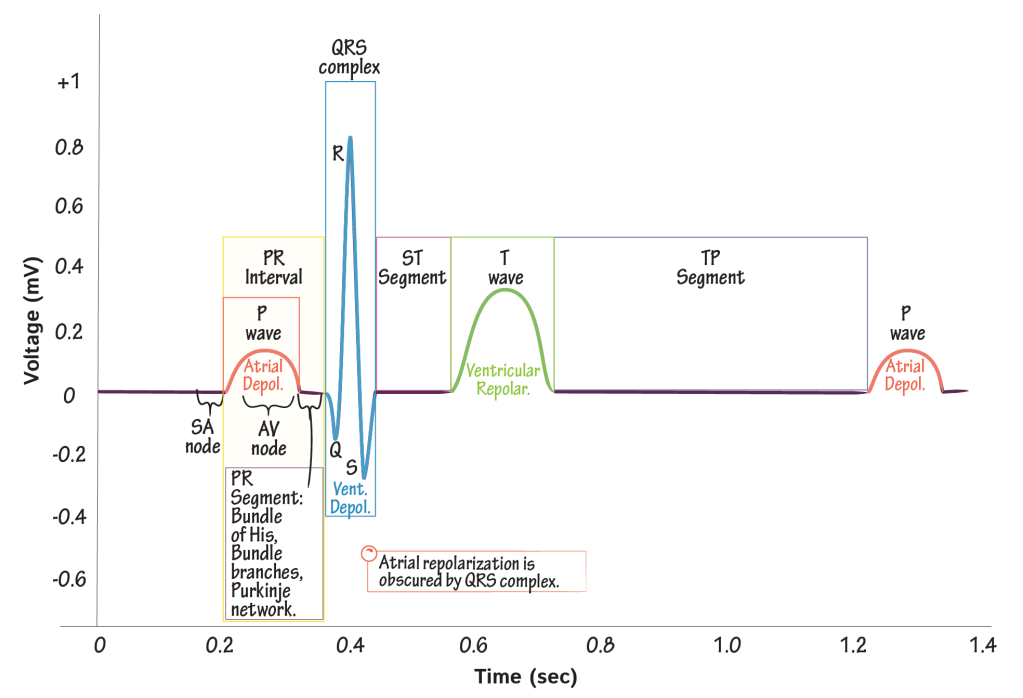
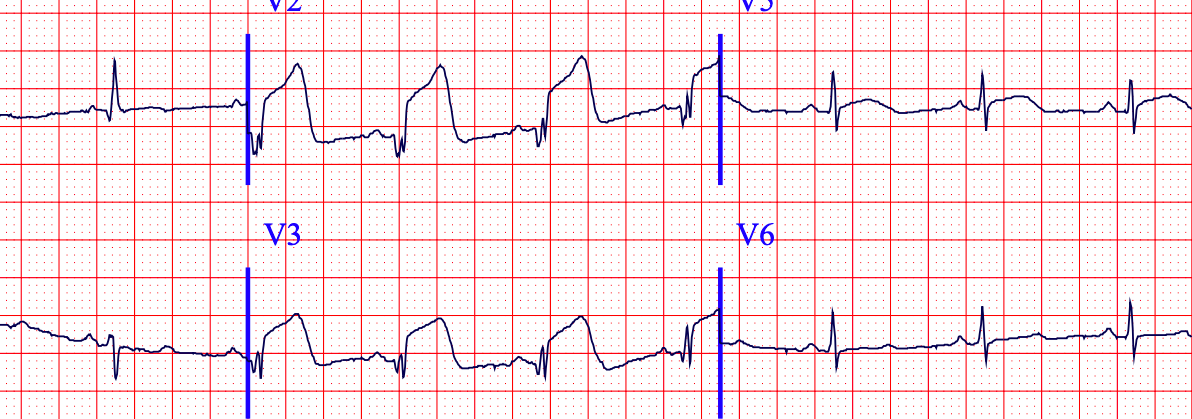
In a STEMI, this ST segment becomes elevated.
Oh-K!
The inciting event leading to ST elevations on an EKG is the inability of mitochondria within ischemic myocardial cells to generate enough ATP, which occurs immediately after the onset of ischemia.
Remember that potassium efflux (i.e., flow out of the cell) is one of the mechanisms by which cardiac myocytes depolarize. One important channel that mediates this flow of potassium is the appropriately named K-ATP channel. It is a potassium exporter that requires ATP to remain CLOSED.
So, when ATP production falls during ischemia, there is less ATP available to keep the K-ATP channel closed and it remains open. As a result, during ischemia more potassium is exported from the myocyte. More potassium export in ischemic cells leads to faster ventricular depolarization of those cells relative to non-ischemic, well-perfused myocytes. The electrical cycle in ischemic cells becomes shorter, which in effect creates an electrical charge difference between ischemic and non-ischemic areas of the heart during depolarization.
As a result of the difference in charges there is a relative current (i.e., flow of charge). In this case the current flows from ischemic to non-ischemic myocardium.
Let’s elevate the discussion
In order to understand why the above leads to ST elevations, it helps to briefly review the conventions for EKG tracings. If charge flows toward a lead, the tracing will deflect upwards. If charge flows away from a lead, the tracing will deflect downwards.
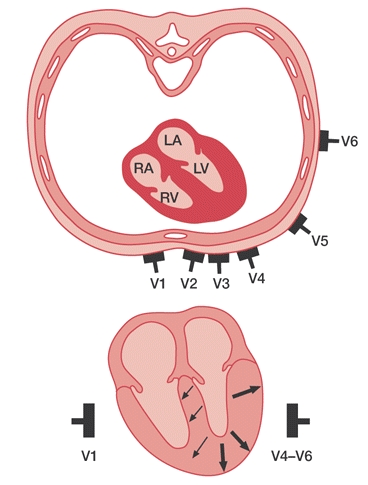
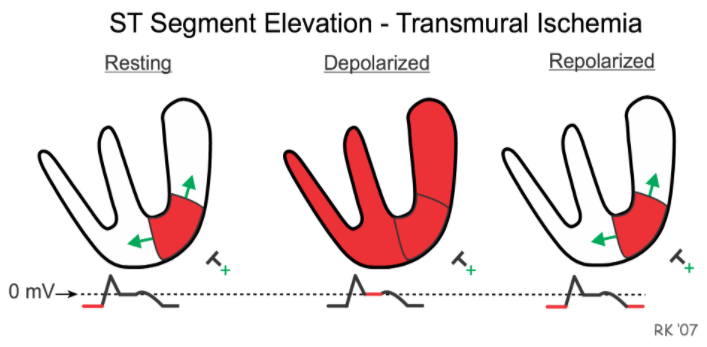
Returning to STEMIs, because there is faster depolarization in the ischemic myocardium, the relative electrical current will flow from ischemic to non-ischemic myocardium. In the leads that are over the ischemic myocardium, this is “away” from those leads since the ischemic area involves all of the myocardium under the lead up to the epicardium (remember, in a STEMI the ischemia is transmural).
This shifts the EKG in a negative direction (i.e., it is depressed on the tracing).
Because there is essentially no difference in repolarization speeds in ischemic and non-ischemic myocytes, once the EKG arrives at this section the gradient disappears and the EKG shifts back upward.
What we are left with is the following explanation for ischemic ST elevations: the ST segment only appears elevated because the baseline of the other EKG segments has been shifted down.
What about subendocardial ischemia…
With subendocardial ischemia (e.g., with an NSTEMI), the mechanism works exactly the same way. Remember that STEMIs involve transmural ischemia where there is no normal, non-ischemic tissue between the ischemic myocardium and the electrodes on the skin. As a result, the ischemic current flows away from the electrode lowering the baseline on EKG and the appearance of ST elevation on EKG.
With subendocardial ischemia (aka non-transmural), there is some non-ischemic tissue between ischemic myocardium and the EKG electrodes. This results in the opposite result finding on EKG. The ischemic current flows toward the electrode, shifting the EKG baseline up and the ST segments appear depressed.

…and hyperacute T waves?
Hyperacute T waves are broad-based, tall T waves of increased amplitude that represent the first signs of ischemia, even before ST depressions or elevation. They are also thought to reflect changes in the speed of depolarization during ischemia due to alterations in the function of the K-ATP potassium channel, similar to ST elevations.
This was investigated in an experiment in dogs in the 1990s where an epicardial artery was occluded after the dogs received either placebo or a specific inhibitor of K-ATP. The animals who received placebo had immediate hyperacute T waves on EKG. Those who got the K-ATP inhibitor had significantly less increase in the amplitude of T waves with ischemia. This suggests that this K-ATP channel plays a key role in hyperacute T waves as well.
Dr. Mike Todorovic (@drmiketodorovic) made a terrific video explaining this mechanism. Worth a watch!
Take Home Points
- Ischemia decreases ATP production, which leads to faster potassium export through the K-ATP channel. This increased potassium export leads to faster depolarization of ischemic tissue, creating a current between ischemic and non-ischemic myocardium.
- In transmural myocardial infarctions, which cause STEMIs, this current is directed away from the EKG leads on the skin resulting in a lower baseline on the EKG tracing.
- Because there is no difference in the speed of repolarization the charge gradient and current stops during this phase of the cardiac cycle. This leads to an isoelectric ST segment, but because the baseline of the tracing was shifted down the ST segment appears elevated.
- The same principles apply for ischemic ST depressions and hyperacute T waves.
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (1.00 hours), Non-Physician Attendance (1.00 hours), or ABIM MOC Part 2 (1.00 hours).
Listen to the episode
Credits & Citation
◾️Episode written by Avi Cooper
◾️Show notes written by Tony Breu and Avi Cooper
◾️Audio edited by Clair Morgan of nodderly.com
Cooper AZ, Abrams HR, Breu AC. Why do myocardial infarctions cause ST elevation? The Curious Clinicians Podcast. March 3, 2021.
Image credit: https://ecg.bidmc.harvard.edu/maven/dispcase.asp?rownum=90&ans=1&caseid=91
Related tweetorial: https://x.com/AvrahamCooperMD/status/1208154632892993536

Mind blown. I’m a lowly full time firefighter/paramedic, inactive RN, but I teach a lot. Never have I ever heard this. Thanks for the info. I’m so glad to have found this site!
LikeLike
Similar mechanism for STE during LBBB, LVH, V-tach??
LikeLike
isnt it completely wrong?
as far as i know, K+ efflux causes repolarization NOT depolarization
LikeLike
Yes under normal circumstances, but in myocardial ischemia there is inadequate blood supply to the myocardial tissue leading to anaerobic metabolism and this impairs ATP production. ATP being responsible for regulating the potassium channels. Is significantly less present leading to effectively wide open potassium channels. So you have an ever increasing amount of extracellular potassium, and now potassium starts accumulate within myocyte and becomes more positive earlier in the cardiac action potential ,which triggers early depolarization.
LikeLike