Why do we use urinary antigen tests for respiratory pathogens?
For many pulmonary infections, we look at the urine to make a diagnosis. This is true for bacterial causes like strep pneumonia and legionella, and also for some fungal infections like Histoplasma. To some extent, this may make sense. Many of us learn early in our training that a good sputum sample is hard to obtain. Maybe this explains why many respiratory infections are not diagnosed via this route. But it doesn’t explain why we don’t simply test the blood.
A simple explanation would be that these infections also target the kidney and evidence of them appears in the urine. But, although some of the infections diagnosed via urinary antigens do involve the kidney (e.g., Legionella) most do not.
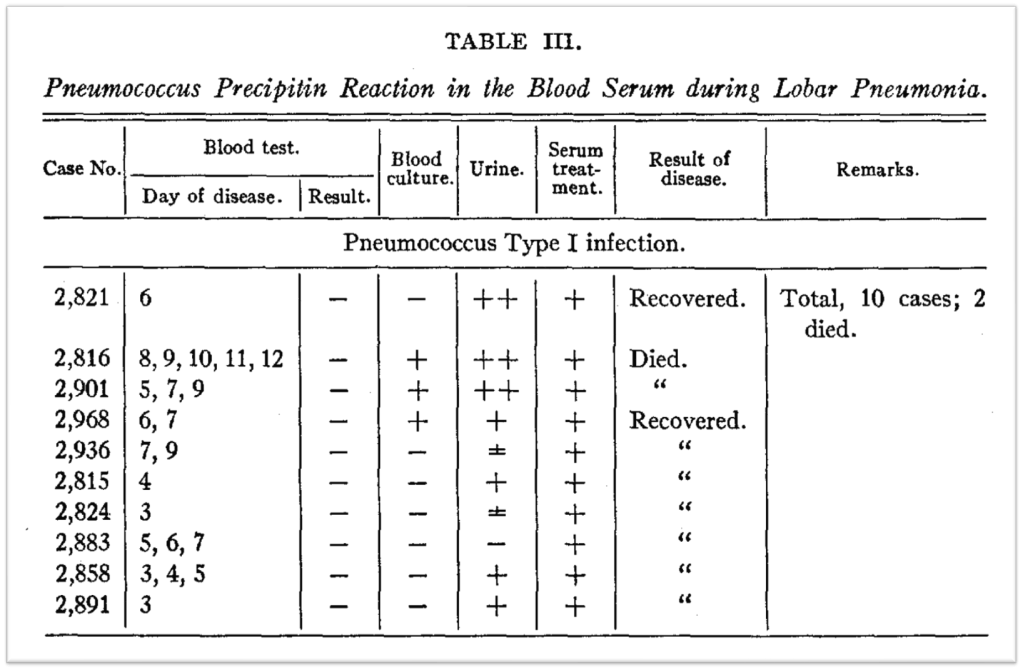
In 1917, Alphonse Dochez and Oswald Avery1 observed that a pneumococcal antigen was readily identified in the urine of patients with lobar pneumonia, even when it couldn’t be isolated in the blood. The antigen Dochez and Avery were studying is the C-polysaccharide of strep pneumoniae.
The studies on the antigen in pneumococcal pneumonia raise two key questions. First, how did the strep antigen gets into the urine if pneumococcus doesn’t itself infect the genitourinary system? Second, if the antigen gets into the urine via the blood, why isn’t the blood test always positive too?
Understanding the answers to these questions requires discussion of the sieving coefficient. The filtration of molecules by the glomerulus is typically quantified using the following ratio:
Concentration in the filtrate / Concentration in the plasma
This is known as the sieving coefficient. The smaller the molecule, the higher the sieving coefficient, meaning more of it is filtered. As an example, sodium has a sieving coefficient of 1.0. We know this as it is freely filtered given its small weight (0.02 kDa) and molecular radius (0.1 nm). It is tiny.

Albumin, on the other hand, has a sieving coefficient of <0.01. This is partly a reflection of both the size of the albumin at 69 kDa and 3.55 nm (i.e., it is >3000 times as heavy as sodium and has a radius 35 times as wide). But we also know that charge plays a role. Albumin is negatively charged and so are the endothelial cells of the glomerular basement membrane. This makes it even harder for albumin to pass through the glomerulus. But a negatively charged molecular that is small enough will still have a sieving coefficient of 1.0. One example is chloride.
In order to establish that the antigens used to diagnose legionella and strep are filtered, it’ll help to know their sieving coefficient. These values are not readily available but can be estimated based on the size of the molecules. The molecular weight of C-polysaccharide is about 22 kDa, roughly half that of albumin. A reasonable comparator is myoglobin which has a molecular weight of 17 kDa. And, myoglobin has a sieving coefficient of 0.75. This is why rhabdomyolysis can lead to tubular injury – some myoglobin is able to cross the glomerulus and access the tubules.
Notice that the sieving coefficient is not the same thing as fractional excretion. Simply because a molecule is freely filtered does not meet it will make its way into the urine. Again, sodium and chloride provide good examples as their fractional excretions are not 100%. In fact, they are closer to 1%. Once these antigens are filtered, it appears that they are not significantly reabsorbed or excretion. You might say the fractional excretion of the strep urinary antigen is 100%.
Regarding the second question (if the antigen gets into the urine via the blood, why isn’t the blood test always positive too?), this is important because it would it is often easier to send a blood test.
A clue comes from another freely filtered polysaccharide: inulin. Inulin is a carbohydrate, like C-polysaccharide. And it’s pretty small at 5 kDa. If we assume that these two carbohydrates are handled similarly by the kidney, then the relative plasma and urine concentrations of inulin might provide a guide for C-polysaccharide. The urine concentration of inulin is about 440 mg/L. For the plasma, it is 10 mg/L.
It is possible that small microbial polysaccharide antigens have similar relative concentrations. The result might be a positive urine test with a negative blood test. There are a number of reasons why the blood level may be low, including low antigen production, binding of antigens by serum antibodies, sequestration into the reticuloendothelial system, and antigen metabolism.
It is worth noting that many other infections also have available urinary antigen tests. These include leishmaniasis, malaria, tuberculosis, Leprosy, Chagas disease, and endemic mycoses beyond histoplasma.
As a final note, there is data suggesting that some urine antigens are degradation products. Presumably because of the slow breakdown of polysaccharides in mammalian tissues and the large load of antigen deposited during an infection – several grams in the lungs in pneumococcal pneumonia – urinary excretion of polysaccharide antigens can persist for many days or weeks. There is even a case report of a urine legionella antigen persisting for 326 days after infection. And going back to Dochez and Oswalt, in their original paper from 1917, they report three patients who had recovered from pneumococcal pneumonia and who still excreted pneumococcal polysaccharide at 40, 42, and 58 days after the onset of their illnesses.
Take Home Points
- Many urinary antigens are small, with high sieving coefficients.
- This leads to their presence in the urine at high concentrations, even if the organism isn’t in the urine.
- Serum concentrations may remain low.
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (1.00 hours), Non-Physician Attendance (1.00 hours), or ABIM MOC Part 2 (1.00 hours).
Listen to the episode
https://directory.libsyn.com/episode/index/id/23072861
Credits & Citation
◾️Episode and show notes written by Tony
◾️Show notes written by Avi Cooper and Tony Breu
◾️Audio edited by Clair Morgan of nodderly.com
Breu AC, Cooper AZ, Abrams HR. Urine the Lung. The Curious Clinicians Podcast. May 11, 2022.
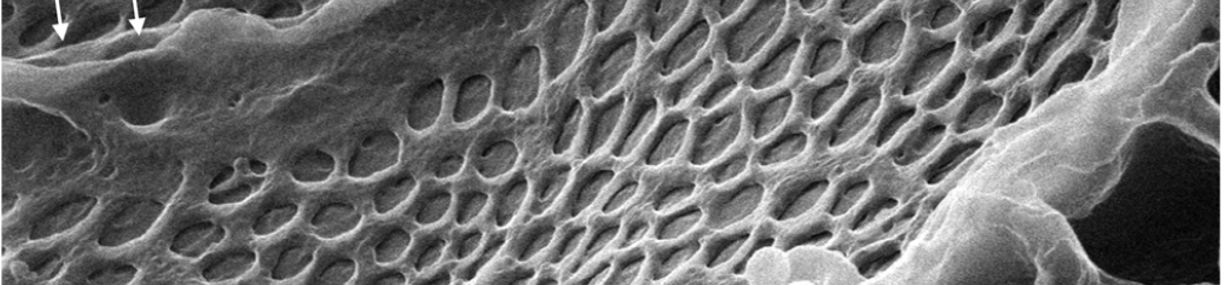
Image credit: Evaluation of the Glomerular Filtration Barrier by Electron Microscopy, Modern Electron Microscopy in Physical and Life Sciences. DOI: 10.5772/61811.
1Yes, this is the same Oswalt Avery that identified DNA as the stuff of genes, though that work was done decades later.
2C-polysaccharide is what CRP “reacts” with, giving it its name, C-reactive protein.