For this episode, Avi reached back to a memory of a teaching conference given by a co-resident during internal medicine residency: furosemide works by non-diuretic mechanisms in the acute setting, providing immediate relief to patients with acute pulmonary edema even before an increase in urine output.
Furosemide was introduced as a loop diuretic in 1964 and its use in acute congestive heart failure and pulmonary edema was described in a case series soon thereafter. The authors observed that treatment of pulmonary edema with furosemide led to a quick improvement in dyspnea, often before diuresis.

Where’s the data?
There is data supporting an immediate effect with furosemide beyond patients’ subjective reports of feeling better. A 1974 study measured left ventricular (LV) filling pressures after intravenous furosemide administration. Not surprisingly LV filling pressures decreased with a peak effect at about 15 minutes. But they also found that the decrease in LV filling pressures began very early: within 5 minutes.

The earliest physiologic change that the group detected was a dramatic increase in venous capacitance, also within about 5 minutes. This implied that furosemide caused rapid-onset venodilation. This correlated exactly with the drop in filing pressures that they found, further suggesting venodilation as the cause. Urine output didn’t begin in earnest until about 30 minutes after administration, so it wasn’t the diuretic effect of furosemide that led to these findings.

What leads to venodilation?
The first clue to the mechanism of furosemide-induced venodilation came in an experiment in dogs in the 1970s. The researchers made them simultaneously hypervolemic and also anuric by ligating the ureters. They then administered furosemide and – as you’d expect from the study above – pulmonary capillary wedge pressure decreased. Again, this was despite their inability to make urine.
The investigators then pre-treated the dogs with indomethacin (an NSAID) before furosemide and again measured filling pressures. Indomethacin blunted the effects of furosemide as the wedge pressure did not decrease.

Because NSAIDs, including indomethacin, inhibit cyclooxygenase-1,2, they block production of prostaglandins. Although prostaglandins have many physiologic effects, for our purposes it is important to remember that they are potent vaso/venodilators. This experiment implicated prostaglandins as the mediators of furosemide-induced venodilation.
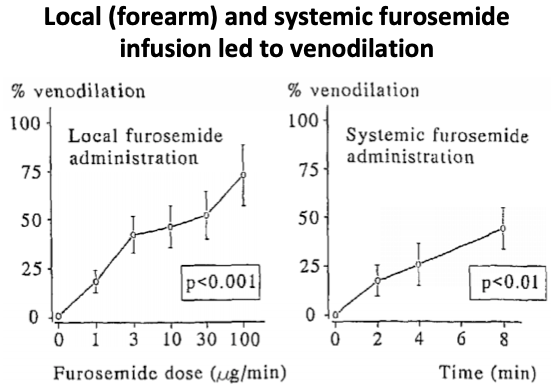
There are additional studies strongly supporting this mechanism. A 1997 study looked at furosemide’s effect on vascular tone in the forearm. In particular, arterial and venous blood flow was recorded after furosemide infusion. While arteries didn’t react, veins dilated up to 72%. This venodilatory effect was blocked by indomethacin, implicating prostaglandins directly.
As to how furosemide impact prostaglandins, it seems to directly increase prostaglandin release from endothelial cells. This was studied in cultured bovine aortic cells in the 1990s, where addition of furosemide led to a 3-fold increase in prostaglandin production within a couple of minutes of incubation. The exact mechanism is not clearly defined, but there is some recent evidence that it may inhibit the effects of prostaglandin dehydrogenase, which breaks down and inactivates prostaglandins. So perhaps there are more prostaglandins around with furosemide because it blocks degradation.
What about other effects?
Inhaled furosemide has been studied in dyspnea palliation for cancer patients and shown to be efficacious. The mechanism isn’t well understood but may involve modulation of j-receptor signaling. But, if furosemide increases prostaglandin activity, it should act as an indirect bronchodilator. And that’s exactly what seems to happen based on an experiment in rat airways. Treatment with methacholine and serotonin provoked bronchoconstriction, and furosemide was able to block the effects of those bronchoconstrictors – effectively inducing bronchodilation. Incredibly, similar to the venodilation studies, pre-treatment with indomethacin blocked furosemide’s ability to bronchodilate.


Take Home Points
- Furosemide rapidly decreases left ventricular filling pressures in acute heart failure and does so via venodilation.
- The mechanism for venodilation is upregulation of prostaglandins in the endothelium.
- Furosemide also acts as a bronchodilator via the same mechanism
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (1.00 hours), Non-Physician Attendance (1.00 hours), or ABIM MOC Part 2 (1.00 hours).
Listen to the episode
Credits & Citation
◾️Episode written by Avi Cooper
◾️Show notes written by Tony Breu and Avi Cooper
◾️Audio edited by Clair Morgan of nodderly.com
Cooper AZ, Abrams HR, Breu AC. Why can furosemide improve pulmonary edema from heart failure almost immediately? The Curious Clinicians Podcast. May 12, 2021
Image credit: http://www.emdocs.net/furosemide-treatment-acute-pulmonary-edema/
Related tweetorial: https://x.com/AvrahamCooperMD/status/1292134482812604418?lang=en