Why do patients with methemoglobinemia have an oxygen saturation fixed at 85%?
Here’s a case for you: an older patient with lung cancer undergoes an awake intubation with benzocaine. They then experience hypoxemia which stays fixed at 85% despite receiving 100% FiO2 oxygen. The care team does an ABG, which yields chocolate-colored blood with a PO2 of 284. Diagnosis?
Methemoglobinemia! This patient’s methemoglobin level came back elevated at 24%, and their hypoxemia resolved with the administration of methylene blue.
A pretty classic board question. However, because we’re the Curious Clinicians, we have more questions, three to be precise. What exactly is methemoglobinemia? Why is the O2 saturation fixed at 85%? And why are patients at such a high risk of cyanosis despite that not-terrible O2 saturation and high PO2?
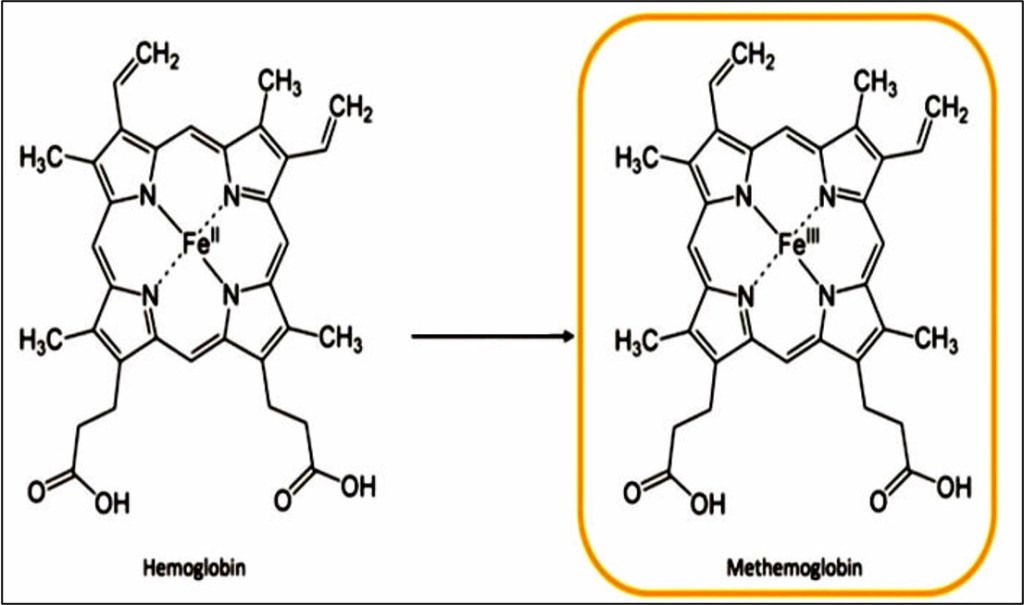
Methemoglobinemia involves, unsurprisingly, methemoglobin. Normal hemoglobin in human red blood cells (RBCs) contains four heme groups, each containing a “ferrous” iron in the 2+ configuration. This “reduced” charge is “oxidized” to 3+ when exposed to oxidizing agents, like metabolites of the benzocaine spray that our patient received. Hemoglobin that contained 3+ “ferric” iron is called methemoglobin.
Methemoglobin is not, in and of itself, toxic. However, it disrupts normal oxygen delivery in two ways. First, 3+ ferric iron is a poor binder of oxygen, so methemoglobin has a poor O2-carrying capacity compared to normal hemoglobin. By itself, this wouldn’t be too much of a problem, because not every iron within the hemoglobin tetramer is oxidized when exposed to a culprit agent. However, ferric heme can cause normal, ferrous heme to dramatically increase its affinity to oxygen. This is a deadly combination: RBC’s are poor at picking up oxygen from the lungs, and the oxygen they do bind, they bind so tightly that they can’t release it. In a sense, methemoglobinemia is similar to severe anemia – cyanosis is far worse than oxygen saturation would indicate, because delivery, not absorption, of oxygen is the primary problem.
One key feature of methemoglobinemia, though, is that oddly-precise O2 sat of 85%, which gets neither better nor worse with administration of 100% FiO2. To understand why it remains fixed at 85%, we have review how pulse oximetry works. It measures arterial oxygen saturation by analyzing the absorption of light at two different wavelengths. Oxygenated hemoglobin and deoxygenated hemoglobin have different absorption spectra for light. Deoxyhemoglobin is more able to absorb red light with a wavelength of about 660 nm. Oxyhemoglobin is more able to absorb infrared light with a wavelength of about 940 nm. The standard pulse oximeter is an LED that emits both types of light over a vascular bed (usually the finger), measures the ratio of absorbed infrared to red, and converts that ratio to a percentage based on a calibration curve.

Methemoglobin, on the other hand, absorbs the red 660 nm and infrared 940 nm light nearly equally, regardless of its actual oxygen content. For the pulse oximeter, a 1:1 ratio corresponds to an O2 sat of 85%. When treating a patient with methemoglobinemia, it’s vital to remember that the pulse oximeter reading is entirely based on that infrared/red ratio, and therefore that 85% is neither the patient’s actual saturation nor an accurate measure of their tissue oxygen delivery.
Take Home Points
- Methemoglobin is a form of hemoglobin where the iron atom is in the 3+ ferric form, instead of the usual 2+ ferrous form
- Ferric iron does not bind oxygen well. The heme molecules containing ferric iron also lead to changes in the neighboring ferrous iron, leaving them less apt to release their oxygen molecules. Collectively, this leads to horrible oxygen delivery and cyanosis.
- The pulse oximeter is stuck at 85% saturation in methemoglobinemia because both spectra of light are absorbed equally.
Listen to the episode!
https://directory.libsyn.com/episode/index/id/35664635
CME/MOC
Click here to obtain AMA PRA Category 1 Credits™ (0.5 hours), Non-Physician Attendance (0.5 hours), or ABIM MOC Part 2 (0.5 hours).
As of January 1, 2024, VCU Health Continuing Education will charge a CME credit claim fee of $10.00 for new episodes. This credit claim fee will help to cover the costs of operational services, electronic reporting (if applicable), and real-time customer service support. Episodes prior to January 1, 2024, will remain free. Due to system constraints, VCU Health Continuing Education cannot offer subscription services at this time but hopes to do so in the future.
Credits & Suggested Citation
◾️Episode written by Tony Breu
◾️Show notes written by Tony Breu and Giancarlo Buonomo
◾️Audio edited by Clair Morgan of nodderly.com
Breu AC, Abrams HR, Cooper AZ, Buonomo G, . Pulse Check: Methemoglobin. The Curious Clinicians Podcast. March 12th, 2025.
Image Credit: Annals of Emergency Medicine

